Introduction
Many of us are familiar with First Aid. We know what to do when someone injures themselves in an accident or gets sick. But how do we deal with someone who deals with emotional stress or trauma? What are things we have to watch out for and what are common misconceptions about mental illness and Psychological Support? These are some of the topics covered in the three-day online training on Psychological Support, Psychological First Aid and Trauma-Informed Care, facilitated by Fatima Jarrar.
Misconceptions about Mental Illness and Psychological Support
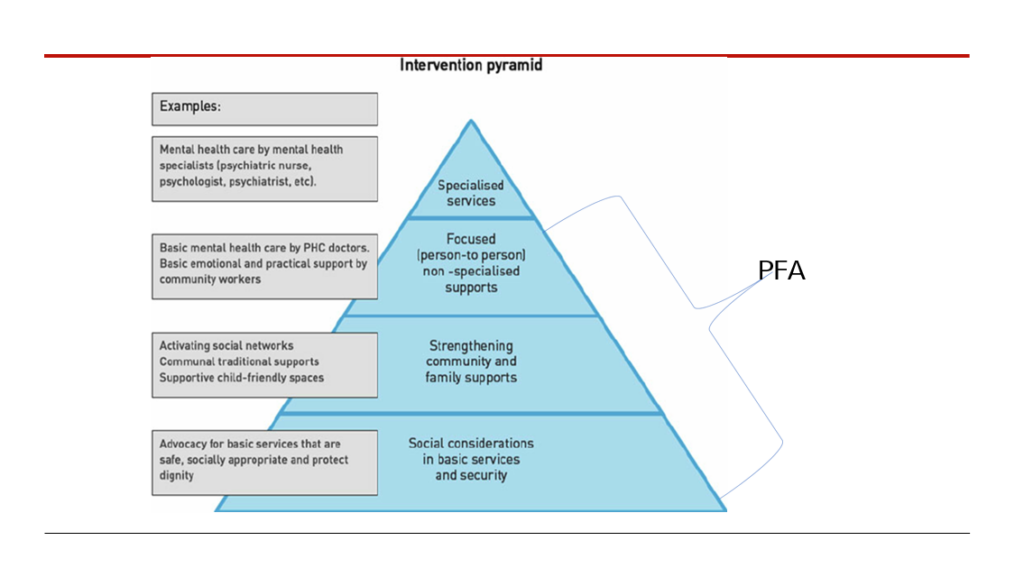
The first step was to address some common misconceptions. We agreed that mental illness is not a personal failure, and neither is it someone being too sensitive, but it is a medical condition that must be taken seriously. Next, we discussed who needs Psychological Support. Psychological Support is not only for people who have a medically assessed mental illness because there is a significant number of people struggling with mental illness but do not have it medically assessed. In addition, we all struggle with forms of mental illness sometimes and deserve Psychological Support. The last important information was that Psychological Support is non-specialized support meaning that it is not professional help. We can try to lend basic support but should refer the beneficiary (person who receives support) to specialized services in serious situations.
How to: Psychological Support
Having addressed misconceptions about mental illness, we got into the practicalities of giving Psychological Support. In interactive role plays where one person offered support and the other one could decide if they wanted to accept, we discussed when we felt most comfortable. Then we compared our findings with the established criteria for good Psychological Support and found some overlap. The main criteria are:
- Confidentiality: Beneficiaries (person receiving support) might want to share sensitive information about themselves and their lives. For them to be able to do so, this information must be kept confidential.
- Communicating Concern: Try to express your empathy and concern by expressing your understanding of the person’s situation.
- Non-verbal Skills: While listening to the person receiving support, we should try to read their body language and, more importantly, use our body language in a culturally appropriate way to express that we are listening.
- Validating: Beneficiaries sometimes discredit their own feelings or assume they are the only ones who face them. Ensuring them that their feelings are valid, and many people have similar experiences is thus crucial for the person receiving support to feel comfortable.
- Putting aside Personal Values: We often engage with people who have fundamentally different values. This should not impact the way we treat them when giving Psychological Support.
- Not giving Advice: When giving Psychological Support we should avoid talking about how we would solve their issue but instead be there to listen to them.
How to: Trauma-Informed Care
On day two, the focus was on Trauma-Informed Care. Trauma Informed Care should be practiced everywhere but is especially relevant for Psychological Support. To provide Trauma-Informed Care we were first learnt what trauma is. When we experience a potentially traumatic experience our brain goes into survival mode shutting down all essential body and mind processes. After the experience the brain usually switches back into normal mode but in some cases, this fails to happen. In this case the affected person has undergone a traumatic experience. Trauma-Informed Care should be done always regardless of whether we know that the beneficiary is traumatized or not. After the introduction to Trauma-Informed Care, we then went through key steps to give support and aid in a way that is Trauma-Informed. At the start, it is important to create a safe environment, build trust and be transparent. While giving care it is important to be compassionate and show empathy. This enables collaboration where care is not forced onto the beneficiary but is a cooperative process between the beneficiary and the supporting person. Lastly it is important to be sensitive towards culture, history and gender to not offend or discriminate against the beneficiary.
How to: Psychological First Aid
On the last day we discussed Psychological First Aid (PFA). And what key points of action are if someone needs immediate PFA. We learned that we should inform ourselves in advance about available services and support as well as other safety and security concerns. In a situation where we are unsure about who needs immediate PFA we should look for people who exhibit serious distress reactions. When we make contact, we should do so in a calming manner and listen to their immediate concerns. We then need to make sure that people’s basic needs are addressed. This can include water and food, but they might also have physical injuries that need treatment. After addressing these basic needs, we can start helping people cope with their experiences that lead to psychological distress. This should be done in an environment where the beneficiary feels safe and comfortable so that they can regain a sense of normality. The last step is to inform them about other services through which they can get specialized support and connect them with loved ones.